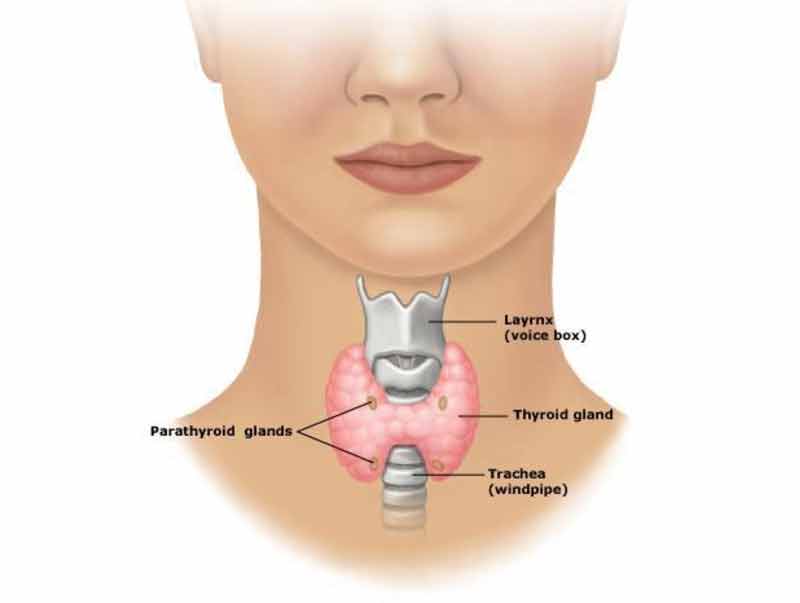
The parathyroid glands
- The parathyroid glands are located in the lower part of the neck on either side of the thyroid gland
- The parathyroid glands produce parathyroid hormone (PTH) which acts to raise the level of calcium in the blood
- Bone cells are very sensitive to PTH and respond by releasing calcium
- If the parathyroid glands are overactive and produce too much parathyroid hormone then the calcium level in the blood rises
- Over months or years the loss of calcium can result in bones that are weak and more likely to fracture
Minimally invasive parathyroidectomy (MIP)
- Parathyroidectomy is the treatment of choice in symptomatic primary hyperparathyroidism
- Minimally invasive parathyroidectomy or minimally invasive parathyroid surgery cures fatigue and the bone, abdominal, urological, and mental symptoms associated with hypercalcaemia – parathyroidectomy also results in a quantifiable improvement in health related quality of life
- Minimally invasive parathyroid surgery is reliable and safe and has become the first line treatment of primary hyperparathyroidism in specialist units in Australia, Europe and the United States
- Minimally invasive parathyroid surgery is possible when an adenoma in one of the parathyroid glands is the cause for hyperparathyroidism
- Minimally invasive parathyroid surgery has a 50% reduction in operating time, a shorter hospital stay, and a comparable clinical outcome with no notable difference in the type or number of complications – when compared with conventional neck exploration in large studies
- Patients with multiple parathyroid gland disease are unsuitable for MIP surgery and require a conventional parathyroid operation
The aims of minimally invasive parathyroidectomy
- After successful minimally invasive parathyroid surgery the PTH in the blood will return to an appropriate level and the calcium levels will return to normal
Anaesthesia for parathyroidectomy
- Minimally invasive parathyroid surgery is routinely performed under general anaesthesia
- The anaesthetic is given by a specialist Anaesthetist
- Modern anaesthesia is safe, however, rarely serious reactions to anaesthesia occur
- If you have ever had a reaction to an anaesthetic drug tell your Anaesthetist and Surgeon
- Your Anaesthetist will be able to explain which anaesthetic is best and the associated risks and benefits
Incision for minimally invasive parathyroidectomy
- A horizontal skin incision is made in one of the lower neck skin creases over the culprit parathyroid gland
- The incision is usually around 2cm long and is closed with dissolving sutures and then taped with micropore
- With routine wound care including taping in the early post-operative period the scar usually settles to blend in with the skin creases
Recovery after minimally invasive parathyroidectomy
- Minimally invasive parathyroid surgery is usually performed as a day stay or overnight stay procedure
- Most people recover fairly quickly after minimally invasive parathyroidectomy and resume normal activities within one week
- A post-operative visit at two to three weeks is routine to review the results. You will need to contact the office to make an appointment for that visit
Follow-up after parathyroid surgery
Generally follow-up will consist of:
- A visit at 2 to 3 weeks for a wound check. You will need to contact the office to make an appointment for that visit
- Α final surgical review at 3 months
- Patients who require calcium supplements need to be seen by the Local Doctor on a weekly basis to have the blood calcium level checked and to have the calcium supplements progressively reduced
- Endocrinology review is needed 2 to 3 months after surgery for progress monitoring
- Your Local Doctor or Endocrinologist may need to see you more frequently for if there are any problems
Calcium supplements
- After successful parathyroid surgery the calcium level falls to normal very quickly
- A temporary drop in calcium levels below normal also sometimes occurs
- Symptoms of a low calcium level may include tingling around the mouth and in the hands, and, cramping (“tetany”) of the hands and feet
- Patients with a low calcium level after parathyroidectomy are usually sent home on calcium supplements and will need to see their Local Doctor every week to have the calcium levels monitored and calcium supplements reduced accordingly
- Following parathyroid surgery, if there are any concerns or problems, speak to your Local Doctor, who will arrange to contact your Surgeon
If you have any queries about minimally invasive parathyroid surgery please contact your local doctor who will arrange to contact your thyroid surgeon