
From 1997 to 2006, mortality rates remained unchanged in NSW and the survival rate was high – the five-year survival is 89% in males and 95% in females (overall the survival rate for people with thyroid cancer is 98% when the disease is localised at diagnosis).
Thyroid cancer causes
As with many types of cancer, a family history is a known risk factor. A family history carries the biggest risk for patients with first degree relatives. About 5% of patients who develop papillary thyroid cancer and 20-25% of patients who develop medullary thyroid cancer (MTC) will have a relative who also had thyroid cancer.
Thyroid cancer detection and screening
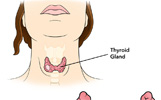
 Doctors screen by examining the thyroid gland, to check for a lump or nodule. If a doctor feels a nodule, it does not mean cancer is present. Most thyroid nodules are not cancer.
Doctors screen by examining the thyroid gland, to check for a lump or nodule. If a doctor feels a nodule, it does not mean cancer is present. Most thyroid nodules are not cancer.
Types of thyroid cancer
 There are 4 main types of thyroid cancer, and some are more common than others. Cancer types and incidence include: Papillary and/or mixed papillary/follicular cancer 80%; Follicular and/or Hurthle cell cancer 15%; Medullary thyroid cancer 3%; Anaplastic thyroid cancer 2%.
There are 4 main types of thyroid cancer, and some are more common than others. Cancer types and incidence include: Papillary and/or mixed papillary/follicular cancer 80%; Follicular and/or Hurthle cell cancer 15%; Medullary thyroid cancer 3%; Anaplastic thyroid cancer 2%.
Papillary thyroid cancer
 Papillary carcinoma of the thyroid is the most common cancer of the thyroid gland. Cancer usually begins as a small lump (nodule) in the thyroid gland, which is located at the center part of the front of the neck.
Papillary carcinoma of the thyroid is the most common cancer of the thyroid gland. Cancer usually begins as a small lump (nodule) in the thyroid gland, which is located at the center part of the front of the neck.
Follicular thyroid cancer
 Follicular carcinomas are the second most common type of thyroid carcinoma. Follicular thyroid carcinoma (FTC) is a well-differentiated tumour. In fact, FTC resembles the normal microscopic pattern of the thyroid.
Follicular carcinomas are the second most common type of thyroid carcinoma. Follicular thyroid carcinoma (FTC) is a well-differentiated tumour. In fact, FTC resembles the normal microscopic pattern of the thyroid.
Hurthle cell thyroid cancer
 Hurthle cell cancer is usually classified with follicular thyroid cancer, although it is a distinct and uncommon type of thyroid tumour.
Hurthle cell cancer is usually classified with follicular thyroid cancer, although it is a distinct and uncommon type of thyroid tumour.
Medullary thyroid cancer
 Unlike papillary and follicular thyroid cancers which arise from thyroid hormone producing cells, medullary cancer of the thyroid originates from the parafollicular cells (also called C cells) of the thyroid.
Unlike papillary and follicular thyroid cancers which arise from thyroid hormone producing cells, medullary cancer of the thyroid originates from the parafollicular cells (also called C cells) of the thyroid.
Anaplastic thyroid cancer
 The major problem with anaplastic thyroid carcinoma is that it is usually too aggressive and invasive when it is diagnosed.
The major problem with anaplastic thyroid carcinoma is that it is usually too aggressive and invasive when it is diagnosed.
Thyroid cancer treatment
 Surgery is the most common treatment for thyroid tumours. I131, thyroid hormone therapy, targeted therapy, radiotherapy, and chemotherapy may also be used to treat thyroid cancer.
Surgery is the most common treatment for thyroid tumours. I131, thyroid hormone therapy, targeted therapy, radiotherapy, and chemotherapy may also be used to treat thyroid cancer.
Radioactive iodine
 The radioactive form of iodine (I-131) is often used to treat hyperthyroidism and thyroid carcinoma, and in small doses, to test thyroid function. Iodine is a natural substance your thyroid uses to make thyroid hormone. Radioactive iodine (RAI) is collected by your thyroid gland in the same way as non-radioactive iodine.
The radioactive form of iodine (I-131) is often used to treat hyperthyroidism and thyroid carcinoma, and in small doses, to test thyroid function. Iodine is a natural substance your thyroid uses to make thyroid hormone. Radioactive iodine (RAI) is collected by your thyroid gland in the same way as non-radioactive iodine.
Prognosis for patients with thyroid cancer
 The prognosis for patients with thyroid cancer depends on many factors including: The tumour type; The age of the patient and gender; The local and regional tumour extent at the time of diagnosis; Spread of the tumour into the adjacent structures in the neck; Spread or metastasis of the tumour to other areas of the body.
The prognosis for patients with thyroid cancer depends on many factors including: The tumour type; The age of the patient and gender; The local and regional tumour extent at the time of diagnosis; Spread of the tumour into the adjacent structures in the neck; Spread or metastasis of the tumour to other areas of the body.
If you have any questions about thyroid symptoms or thyroid surgery, you should speak to your local doctor, who will arrange to contact your thyroid surgeon.

