About Hyperthyroidism
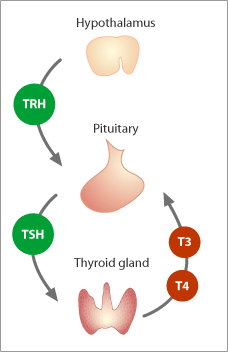
The thyroid is an important endocrine gland in the body. It produces the hormones necessary to maintain homeostasis, or, a constant internal state. The thyroid produces thyroid hormones, T3 and T4, which control energy metabolism and generation of body heat, amongst other functions.
The thyroid gland also produces calcitonin, a hormone which regulates the levels of calcium within the circulation. Hyperthyroidism is a condition where the thyroid gland produces an excessive quantity of thyroid hormones; meaning the gland is over-active.
People with hyperthyroidism experience a number of signs and symptoms, which include unexplained weight loss, constantly feeling hot (especially when others are not), excessive sweating, menstrual irregularities, heart palpitations and diarrhoea. There are a number of causes for hyperthyroidism. Graves’ disease is the most common cause of hyperthyroidism. Other causes for the condition include thyroid nodules and inflammation of the gland. It is also possible for women to develop hyperthyroidism after giving birth.
Graves’ Disease
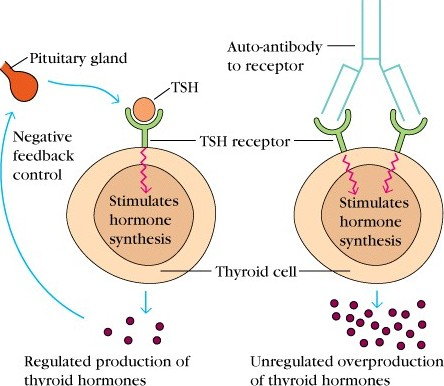
Graves’ disease is an autoimmune condition which is found in approximately 1% of the population. It affects 8 times more women than men, and most commonly occurs during middle age (1). In Graves’ disease, IgG antibodies are produced against the thyrotropin receptor, to which thyroid stimulating hormone (TSH) binds (2).
The antibodies mimic the normal action of TSH; to stimulate the thyroid gland to produce and release thyroid hormones. This is achieved by promoting the uptake of iodide into the cell, promoting the synthesis of thyroglobulin, a thyroid hormone precursor, and by promoting the release of T3 and T4 from the thyroid gland (3).
The constant stimulation of the thyroid gland results in excessive release of T3 and T4 from the thyroid gland. In addition, several changes occur to the cells of the gland itself. The follicular cells increase in size (hypertrophy) and in number (hyperplasia).
The cell height of individual follicular cells also increases, and the amount of colloid (a fluid-like material which contains pre-cursors for thyroid synthesis) decreases (2). As a result of the cellular changes occurring to the cells of the thyroid, the overall size of the gland enlarges and produces goitre. Goitre is a term used to describe an enlarged thyroid gland.
The autoantibodies do not just affect the thyroid gland. In some patients with Graves’ disease, the autoantibodies can affect other organs and tissues in the body. The antibodies especially affect the soft tissues within the eye, causing inflammation and swelling, giving the eyes a bulging appearance. The bulging is also referred to as exophthalmos. It may seem odd that the same antibodies which affect the thyroid can also attack the eyes. This has been explained by proteins within the muscles and fat of the eye which are structurally similar to the TSH receptor (4).
Thyroid Nodules
Thyroid nodules are lumps which are found on the thyroid gland. Approximately 5% of the population have thyroid nodules which can be palpated through the skin. Studies using more reliable detection measures have found this rate to be much higher. Studies using ultrasound technology detect thyroid nodules in about 25% of people. Other studies finding thyroid nodules in as many as 50% of people. Thyroid nodules can be either benign or malignant. Thyroid nodules are more likely to be benign than malignant, with only 5% of thyroid nodules being found to be malignant (5). Patients who have been exposed to radiation to the head and neck region have an increased likelihood of thyroid nodules being malignant (6).
Many thyroid nodules do not produce any symptoms. However, some thyroid nodules can cause hyperthyroidism. Toxic multinodular goitre presents with symptoms typical of hyperthyroidism; tachycardia, cardiac arrhythmia, weight loss, sweats and nervousness (7). Multinodular goitre is the second most common cause of hyperthyroidism behind Graves’ disease and is also a cause of thyroid storm (8). Hyperthyroidism in this case is the result of one or more nodules secreting T3 and T4 independently of stimulation of the gland by TSH (9). As the secretion of T3 and T4 is occurring independently of the normal feedback control, the levels of the hormones can reach excessive levels in the bloodstream and cause the symptoms of hyperthyroidism. It is also possible for a single overactive nodule to cause hyperthyroidism (10).
Thyroiditis
Thyroiditis is inflammation of the thyroid gland. Thyroiditis may be the result of an infection, such as with a virus or bacterium, or another irritating stimulus. Hyperthyroidism is often an early sign of thyroiditis. The inflammatory process occurring within the thyroid results in destruction of the tissue which allows the thyroid hormones to leak out of the gland and enter the bloodstream. However, the phase of hyperthyroidism tends to be only temporary; and after a month or two of chronic thyroiditis, an individual will enter a phase of hypothyroidism (10).
Post-Partum Thyroiditis
Post-partum thyroiditis is inflammation of the thyroid gland that occurs within 12 months after a woman gives birth. There are varying patterns of thyroid function associated with post-partum thyroiditis. The individual may experience solely a hypothyroid phase or solely a hyperthyroid phase. Some women experience an initial phase of hyperthyroidism followed by a period of hypothyroidism. Post-partum hyperthyroidism tends to have an eight week duration, as after this timeframe the gland’s stores of thyroid hormone have been sufficiently depleted. The regulation of thyroid hormone is disrupted following pregnancy, leading to uncontrolled release of hormones and hyperthyroidism (11).
There is a strong link between post-partum thyroiditis and detection of thyroid peroxidase auto-antibodies in the serum. Around 10% of women are found to have the antibodies at approximately 16 weeks gestation. Studies have found that the women without the antibodies present at 16 weeks gestation are highly unlikely to develop post-partum thyroid dysfunction. Whilst a significant number of women with the auto-antibodies present at 16 weeks go on to develop post-partum thyroid dysfunction, the presence of the antibodies does not mean that a woman will experience post-partum thyroid dysfunction (12).
Pituitary Adenoma
A pituitary adenoma is a benign tumour which originates in the pituitary gland. Pituitary adenomas are a very rare cause of hyperthyroidism, accounting for less than 1% of all cases in total. With this in mind, it is an important cause to consider in the patient presenting with thyroid dysfunction.
How exactly does an adenoma in the pituitary gland cause hyperthyroidism? The pituitary gland and the hypothalamus control the actions of the thyroid gland through their release of the hormones TRH (from the hypothalamus) and TSH (from the pituitary). TSH released from the pituitary gland travels in the systemic circulation to the thyroid gland, causing the gland to synthesise and release more thyroid hormone, and to take up more iodine. It is possible for a pituitary adenoma to produce large quantities of TSH, which strongly stimulates the thyroid gland, causing increased production and release of thyroid hormones, resulting in hyperthyroidism.
Hyperthyroidism Treatment
There are several treatments options available for hyperthyroidism exist. The best treatment depends on the specific cause, your age, physical condition and the severity of your condition.
Anti-thyroid medications
These medications gradually reduce symptoms of hyperthyroidism by preventing your thyroid gland from producing excess amounts of hormones. They include propylthiouracil and methimazole. The symptoms of hyperthyroidism usually begin to improve in six to 12 weeks, but treatment with anti-thyroid medications typically continues at least a year and often longer. Results may be temporary or longer lasting. Anti-thyroid medication can cause serious liver damage. Because propylthiouracil has caused far more cases of liver damage, it generally is used when methimazole isn’t tolerated. A small number of people who are allergic to these drugs may develop skin rashes, hives, fever or joint pain. They also can make you more susceptible to infection.
Radioactive iodine
Taken by mouth, I131 is absorbed by your thyroid gland, where it causes the gland to shrink and the symptoms to subside, usually within three to six months. Radioactive iodine has been shown to be generally safe. Because this treatment causes thyroid activity to slow considerably – hypothyroidism usually results. So you will probably need to take thyroid hormone replacement medication every day.
Beta blockers
These drugs are commonly used to treat high blood pressure. They won’t reduce your thyroid levels, but they can reduce a rapid heart rate and help prevent palpitations. Your doctor may prescribe them to help you feel better until your thyroid levels return to normal.
Surgery – thyroidectomy
If you’re planning pregnancy or otherwise can’t tolerate anti-thyroid drugs and don’t want radioactive iodine therapy, you may be a candidate for thyroid surgery. For patients who have unsuccessful medical management, thyroidectomy is a safe procedure which provides excellent results.
If you have questions or concerns about hyperthyroidism see your local doctor who will arrange for you to see a thyroid surgeon.
References
- State Government of Victoria. (2011). Thyroid – Hyperthyroidism. Better Health Channel. link
- Barrett K.E., Barman S.M., Boitano S., Brooks H.L. (2012). Chapter 19. The Thyroid Gland. In K.E. Barrett, S.M. Barman, S. Boitano, H.L. Brooks (Eds), Ganong’s Review of Medical Physiology, 24e.
- McKenna, T. J. (2001). Graves’ disease. The Lancet. 357: 1793-96.
- McKenzie, E. J. & Mortimer, R. H. (2004). Thyroid Nodules and Thyroid Cancer. Medical Journal of Australia. 180(5): 242-247
- Fitzgerald P.A. (2013). Chapter 26. Endocrine Disorders. In M.A. Papadakis, S.J. McPhee, M.W. Rabow (Eds), CURRENT Medical Diagnosis & Treatment 2013.
- Cooper D.S., Ladenson P.W. (2011). Chapter 7. The Thyroid Gland. In D.G. Gardner, D. Shoback (Eds), Greenspan’s Basic & Clinical Endocrinology, 9e.
- Idrose A.M. (2011). Chapter 224. Thyroid Disorders: Hyperthyroidism and Thyroid Storm. In J.E. Tintinalli, J.S. Stapczynski, D.M. Cline, O.J. Ma, R.K. Cydulka, G.D. Meckler (Eds), Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e.
- Bauer D.C., McPhee S.J. (2010). Chapter 20. Thyroid Disease. In S.J. McPhee, G.D. Hammer (Eds), Pathophysiology of Disease, 6e.
- National Institute of Diabetes and Digestive and Kidney Diseases. (2012). Hyperthyroidism. link
- Thyroid Australia Limited. Post-Partum Thyroiditis. link
- Lazarus, J. H., Hall, R., Othman, S., Parkes, A. B., Richards, C. J., McCulloch, B., Harris, B. (1996). The clinical spectrum of post-partum thyroid disease. The Quarterly Journal of Medicine. 89: 429-435
- Weiss, R. E., Refetoff, S. (2012). Thyrotropin (TSH) secreting pituitary adenomas. link

