About Subacute Thyroiditis
Subacute thyroiditis is an uncommon problem that occurs following a viral infection, such as influenza, coxsackie virus or mumps. Mumps is now very rare in Australia due to the success of vaccination. Subacute thyroiditis is most commonly seen in women, typically aged between 20 and 40. Some women develop subacute thyroiditis following pregnancy. People with underlying autoimmune diseases are more susceptible to subacute thyroiditis, and certain medications can predispose to subacute thyroiditis, including lithium (commonly used to treat bipolar depression) and interferon-α (used for a range of conditions, including leukaemia and hepatitis).
There are many names used to describe subacute thyroiditis, including giant cell thyroiditis, subacute non-suppurative thyroiditis, De Quervain’s thyroiditis and subacute granulomatous thyroiditis.
Signs and Symptoms
The classical symptom of subacute thyroiditis is an intense pain in the neck at the site of the thyroid gland. The pain may also radiate to the jaw and the ears. Coughing and swallowing tend to exacerbate the pain. The affected area is also tender. Other symptoms that may occur include:
- Tiredness
- Hoarseness
- Fever
- Trouble swallowing
- Muscle aches and pain
- Malaise (a general feeling of being unwell)
Diagnosis
Pathophysiology
In subacute thyroiditis, the thyroid gland becomes acutely inflamed and releases the thyroid hormones, T3 and T4, which are stored in the gland. The inflammatory process damages the follicular cells in the gland. The follicular cells are responsible for making T3 and T4, and hence, as the cells are damaged, the ability of the thyroid gland to produce the hormones is greatly reduced.
Typically, there are three stages in subacute thyroiditis:
- Thyrotoxicosis: this is the initial stage, where the thyroid hormones are released from the thyroid gland in large quantities. The levels of T3 and T4 in the blood at this stage are well above normal levels. The duration of thyrotoxicosis is variable, but thyrotoxicosis usually lasts for about 6 weeks, until the stores of T3 and T4 in the thyroid gland have been depleted. It does not normally last any more than 3 months. During this stage, some common complaints include sweating, weight loss, tremor, palpitations (conscious awareness of your heartbeat), diarrhoea, nervousness, irritability, difficulty concentrating and feeling hot.
- Hypothyroidism: following the thyrotoxicosis stage, there is a period of hypothyroidism. In this stage, the stores of T3 and T4 have been exhausted from the thyroid gland, and the follicular cells are not capable of producing more to keep up with the body’s demands. The period of hypothyroidism is variable and depends on the duration of the inflammation affecting the gland. Some of the symptoms that may be experienced in this stage include weight gain, constipation, heavier than usual menstrual bleeding, tiredness, and feeling cold. The hypothyroidism stage is also highly variable. It may continue for as long as nine to fifteen months.
- Euthyroid: in most cases of subacute thyroiditis, the inflammation resolves and the follicular cells are able to return to their normal function. The thyroid hormone levels in the blood return to normal and the symptoms resolve. However, in some people, hypothyroidism is permanent.
Tests
If your doctor suspects that you might have subacute thyroiditis, they will order a series of blood tests. The results of the tests vary depending on whether you are in the thyrotoxicosis stage or the hypothyroid stage.
Thyrotoxicosis
Early in the course of subacute thyroiditis, blood tests are likely to reveal the following:
- Erythrocyte Sedimentation Rate (ESR): the ESR is a marker of the level of inflammation in the body. The ESR is likely to be raised above normal limits
- T4: The level of T4 in the blood is likely to be significantly raised above the normal limits
- Thyroid stimulating hormone (TSH): TSH is likely to be well below normal limits. TSH is released in response to low levels of thyroid hormones, and given that T3 and T4 are both elevated, TSH release will be low
Hypothyroidism
- T4: the level of T4 in the blood is likely to fall below the normal range as the gland has depleted its stores and is unable to synthesise additional thyroid hormone
- TSH: TSH is likely to be elevated beyond the normal range because its release is being stimulated by the low levels of thyroid hormone in the blood
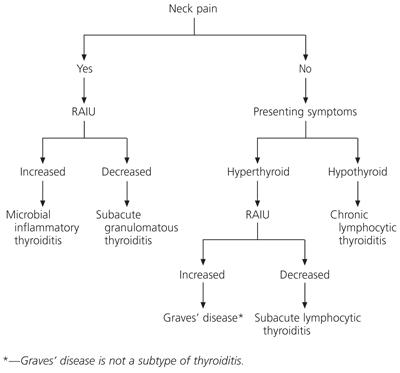
The uptake of iodine is also altered, especially during the thyrotoxicosis phase. During this stage, the damage to the follicular cells means that they are unable to take up iodine as well as usual. Iodine is necessary for the production of thyroid hormones – without it, the hormones cannot be synthesised. The low level of TSH in the circulation during this phase also influences the poor uptake of iodine into the follicular cells. The levels of iodine taken up by the thyroid gland can be measured in a test called the radioactive iodine uptake test. In this test, the patient swallows radioactive iodine either as a liquid or as a capsule. After a few hours, the thyroid gland is scanned to determine the pattern of uptake of the iodine in the gland. It is often scanned about 4 hours after first taking the iodine, and usually again 24 hours later. In subacute thyroiditis, the uptake of iodine is likely to be low in the thyrotoxicosis stage. Uptake is high in Graves’ disease and unequal uptake may be suggestive of a thyroid nodule. This test is not advised during pregnancy and breast- feeding.
Another test that may be performed is to detect the levels of thyroid autoantibodies; these are antibodies produced by the body and act on normal thyroid tissue. These may be mildly raised in people suffering from subacute thyroiditis. If the levels of thyroid autoantibodies are raised significantly, this may be an indicator of an underlying autoimmune cause and a greater likelihood of permanent hypothyroidism.
Treatment
Subacute thyroiditis usually exhibits an excellent response to non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (nurofen). These medications help to relieve the intense pain and can improve some of the other symptoms associated with the condition. If the response to NSAIDs is suboptimal, prednisolone may be required. This steroidal anti-inflammatory drug is generally given for about 3 weeks to help reduce the inflammation. If the symptoms during the thyrotoxicosis stage are problematic, beta-blockers (e.g. propranolol) may provide symptomatic relief. Similarly, if symptoms are severe and/or the hypothyroid phase is prolonged, thyroxine may be required to help stabilise thyroid hormone levels.
If you have questions or concerns about subacute thyroiditis or thyroid health make an appointment to see our thyroid surgeon.

